
|
Paul Sommer's Cochlear Implant Journal
|
Entry #2:
February 4, 2003 (six days after CI surgery)
***WARNING - There are some rather explicit surgical (i.e. bloody) photos below***
Itís been 6 days since my surgery and I finally feel comfortable enough to start writing again.
We (my dad, Sarah, and I) barely arrive in time at Johns Hopkins (due to bad traffic) at 9:30am where we meet my mom (who took train from DC) quickly before meeting with my audiologist. I was anxious to meet my new audiologist since the audiologist I had worked with all along resigned for medical reasons. We take some comfort knowing that my new audiologist, Jennifer Yeagle, is the same audiologist that works with Heather Whitestone, better known as 1995 Miss America. We primarily discuss which processor I should start with. This is one of the biggest decision one must make aside from selecting to go ahead with the surgery and which surgeon/audiologist to work with. I went through several months of doing thorough research on which manufacturer to go with. I choose the Clarion from Advanced Bionics for several reasons, but primarily because of their high sound resolution feature despite the enormous battery drainage. For more info about the differences between the manufacturers, check out: http://www.geocities.com/cicentral/ci_comparison.html.
I'm still in the process of finalizing my decision on which processor to go with. When getting the CI, I automatically get two processors. I have the choice of getting two body-worn processors (BWP), two behind-the-ears (BTEs), or one of each. The choice is made more difficult because Advanced Bionics, the manufacturer of my cochlear implant, is coming out with a new BTE, known as the Auria, this summer, one that I definitely want because of its improved 8-10 hours battery life (the current BTEís battery life is only 4 hours). Jennifer and I agree that Iíd definitely get a ďcertificateĒ for the new BTE known as the Auria, which is expected to come out this summer pending approval from the FDA. But in the meantime, Jennifer gives me another week to think about whether I want to go with the existing BWP or BTE until the Auria comes out. Each of the processors has their own pros and cons. The BWP and the BTE currently on the market have similar features, but there are some pros and cons to each. I will write more later on my decision once I make it by the end of this week.
Itís 10am and we proceed downstairs to the Outpatient Surgical Waiting Room where my name is called within a few minutes. The nurse leads me into the Surgical Prep Room where I change into my gown, have my vitals taken by a nurse, and then receive the IV drip, which will keep me hydrated throughout the surgery. My parents and Sarah are called into the Surgical Prep Room to hang out with me for the next hour or two before I'm called for surgery (which started late due to a prolonged surgery in the room before mine). While Iím in the Barcalounger, a plethora of nurses, anesthesia techs, residents, and fellows come to check on me, ask me various questions, and fill out various forms. They ask me at least 8 times which ear I want to be implanted. I firmly say, ďthe right earĒ every time and could only think of those unfortunate cases of wrong limbs being amputated, etc.
Why the right ear? I have the option of implanting the CI in either ear, especially because my hearing is virtually identical in both ears (as you can see in my audiogram in Entry #1 where X and O represent my left and right ears, respectively. In the earlier years of the CI (which started to become mainstream in the 80s), implanting the worse hearing ear was the norm, especially due to the higher risks then (as CI was then a totally new concept and had been tested little). But nowadays, professionals recommend implanting the better ear because studies show that results are better when using the ear that's been utilized for so many years. After all, the risks of the CI are so minimal now. I choose the right ear for the following reasons:
I'm right-handed; hence, it's more natural for me have the CI on my right ear.
When driving in the car with Sarah, I prefer to be in the driver's seat, so having the CI on my right will prove to be best. It also helps to have the CI on the right, especially if you have the window open in the passenger seat.
Sarah only hears out of her left ear; therefore, compatibility with my wife is best!
My good college baseball teammate/friend (Ryan Isaac) provides another good reason: I bat right-handed - that way, I don't expose my CI side to the pitcher.
My good college roommate/friend (Jon Slemmer), who is currently working towards his PhD in Neuro-Psychology at Cornell, provides another good reason: "language perception and production resides on the left hemisphere of the brain in most people and since everything in and out of the nervous system is flip-flopped, your right ear is more closely wired to your left hemisphere."
The primary nurse then runs over the list of risks involved in the surgery and getting the CI and gives us instructions on post-operative care. The Anesthesia Techs come by and again remind me the risks of anesthesia and explain to me what I should expect once I go into and come out of the operating room. And finally, Dr. Niparko comes by and gives me the final run through the risks and expectations for the surgery and asks me for the last time which ear I want the CI in. In response, he takes his surgical marker and gives me a purple earring on the right ear.

Shortly thereafter, the surgery room is finally cleared and ready for me. I get up and say good-bye to Sarah and my folks then follow the Anesthesia Technician into the Operating Room (OR). Once I get into the room, I take a quick look around and find it to be a familiar environment to the time I worked in the OR in Michigan. I notice the surgeon reviewing my CT scans with his residents and fellows and the nurses putting all the supplies together. The Anesthesia Techs then told me to ďhop on the table.Ē Once on the table, suddenly 4 or 5 people have their hands on me positioning my head and arms, placing electrodes on my chest, etc. Then one of the Anesthesia Techs said, ďRelax, we put the medicine in.Ē Thatís the last moment I recall prior to my "hair cut" and surgery, which started around 1:30pm.
Around 3pm, while I was apparently being ďcleaned up,Ē Dr. Niparko emerged into the Surgical Waiting Room to inform Sarah and my parents that all went very well and presented them with pictures of my implant, which I specifically requested:
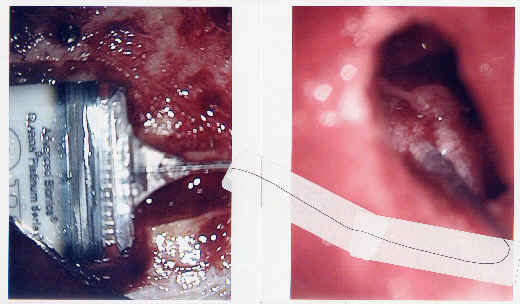
As you can see, the chip is placed with the cord running into the cochlea. For a better "big picture" perspective, check out the picture below (note that this picture below is not of me, but identical to the surgery I had).

As you can see, this picture explains why my scar is so long. Some surgeons have different styles of implanting the CI. I imagine that my surgeon leaves one of the longer scars, but I'm not complaining given his track record. After all, my hair will cover the scar.
Meanwhile, Iím still conked (especially since I apparently required much more anesthesia than the normal patient due to my size) and transported from the OR table to the Recovery Rooms (Phase 1 and Phase 2). I first (at least semi!) consciously wake up in the Phase 2 Recovery Room around 4pm. My first memory is seeing one of the nurses holding up what looked like a cup that one pees into for testing. I recall saying, ďwhy the heck are you asking me to pee now?Ē After consultation with Sarah and my parents, it turned out that the cup actually contained my hearing aids. The nurse asked me if I wanted to put on my hearing aid so I could communicate with him. Had I known that, I certainly would have declined as I was just too conked and felt comfortable relying on lip-reading only at the time.
The next thing I recall (although Iím not sure how much time, if any, passed since the nurse asked me about my hearing aids) is going to the bathroom. I do recall that I felt like throwing up as soon as I got up, rushing to the toilet, and sitting on the toilet trying to throw up. It remains uncertain whether I actually threw up or not. Regardless, it was a bout of nausea. Hence, the nurses immediately gave me very strong cough syrup-like medicine (which I vaguely remember) that knocked me out for another couple of hours.
Finally, I wake up again around 7pm, but feeling much better this time despite continued grogginess. I remember Dr. Niparko stopping by on his way out and giving me a thumbs up informing me that all went very well. I then remember, after some cues later the next day, making some sarcastic comments, which is my way of indicating that Iím okay, to Sarah and my parents. Sarah asked me if I was okay driving to DC and I replied, ďhuh, no, especially not with your driving.Ē Then later responded to a question from my dad saying something to the effect of having my brains leaking through the newly drilled hole in my head. After another hour of dozing in and out, getting dressed, etc., I finally get up again and walk to the car, with the support of the nurses. I slowly get in the car and we are on our way to my momís house in DC.
I barely wake up again and recall my mom and Sarah stopping at Safeway to pick up some feel good vitals, like ginger ale, for me. Then I wake up again right in front of my momís house and remember seeing my momís neighbor, a big guy, come over and help me out of the car and up to my room upstairs in the house. I was then out for another good hour or so before waking up again to my momís Chicken Noodle Soup and toast. This was my first bite in 24 hours. It never tasted so good although I lost some of my taste buds temporarily, which was expected. It feels like I have a burnt tongue.
I crash again immediately after my first post-surgery meal and taking my Tylox (a combination of Oxycodone and Tylenol) and antibiotics. I wake up the next morning (Thursday, Jan 30th) to incredible pain in my neck. My neck has been at the same, uncomfortable, 30-60 degree angle for the last 24 hours. Making matters worse, the anesthesia and drugs make me very weak making it hard for me to move my neck and I could not rest at any other angle for another 24-48 hours except for the few minutes every now and then when I am strong enough to hold my head straight up.
For the whole day (Thursday, Jan 30th) after surgery, I pretty much doze in and out. I cannot take much stimulation. I do not watch any TV at all the next day, only do a very select couple of short emails via my pager from bed, and take a few short zombie-like walks around the house. Sarah and my mom are fabulous nurses treating me to my medicines, food (mostly comprised of soup and toast), and liquids.

But by that evening, I felt much better and ready to have my first visitor, my best childhood friend and best man, Kevin Nolan, Jr. and his girlfriend, Anna. While they visit, I constantly remind Kevin, to little avail, not to make me laugh as it hurts my head. But in revenge, I gross them out because I have a little blood oozing out of my turban and down my neck. After dinner, I quickly fade and say good-bye to the guests. Getting into bed is incredibly painful, especially around my neck because it is sore and my muscles had virtually disappeared; hence, when I strain to put my head down, it turns into throbbing pain. I shook for at least a couple minutes, but felt better after taking more Tylox. I quickly crash shortly thereafter for the night.
Friday morning (Jan 31st) is once again painful on my neck as I slept in one position all night. I feel a bit better later that afternoon after napping all morning. I take a few more short walks around the house. My head itself is virtually numb and felt little pain except for a dull headache. I can definitely feel that I now have a chip in my head and a little wire running down to my cochlea. To those who know me well, the best sign of my recovery occurs on this day as my appetite really starts to come back and I begin eat normally again. Plenty of ice cream and sorbet is the best medicine. The next best sign came when it is time to take off my turban. Sarah carefully and bravely removes my turban to reveal my 9-inch scar for the first time.


I then take my first shower since before the surgery and shampoo my hair, which I did very gingerly and hardly touched the shaved area. Sarah then dresses my scar with hydrogen peroxide and antibiotic ointment, which is now a standard routine twice a day for at least a full week.
Sue Suh, Sarahís best friend from college and maid of honor, comes over for dinner. But I decline to dine with them as I know Sueís energy would wipe me out only in seconds. Sure enough, I crash for the night only minutes after Sue came upstairs to say hi for just a few minutes.
Saturday (Feb 1st) is a much better day as my neck quickly regains strength and becomes more comfortable in that area, but I still spend quite a lot of time in bed. However, it is my first day without taking any naps for the whole day. It is also the first day I no longer take any pain medication although Iím still on antibiotics. I also put on my hearing aids for the first time, but the noise still bother me a bit too much so I quickly took it off again. I pretty much chill around the house and watch the breaking news coverage of the Columbia Shuttle tragedy. The stimulation from the TV is still a bit too much for me. And so is reading.
On Sunday (Feb 2nd), I wake up feeling 75%. I am ready to get out of the house and be on my own again although I did appreciate the spoils of my two favorite nurses! We leave later in the afternoon for Philadelphia where we would split the drive back to Boston with a quick stay-over at my dadís. I put on my hearing aid again and feel comfortable wearing it for a good amount of time. I am also able to talk at a more normal volume after barely mumbling my words in the last few days. We go out for dinner at the pizza restaurant on the first floor of my dadís apartment building, which is a little embarrassing given my terrible haircut and fresh scar (I still cannot quite wear a hat yet in fear of infecting the scar), but people hardly (and thankfully) seem to notice. Later that evening, we get a nice visit from Sarahís parents who dropp by after landing back home at Philadelphia Airport. I think my in-laws, like many others, are a bit taken back by the size of my scar, the concept that I just went in and out on same day for a surgery that involved drilling a hole in my head, and the fact I do not require a follow-up visit to the doctor following the surgery.
We leave early the next day (Monday, Feb 3rd) for Boston. It's was finally good to be home later that afternoon. I am however reminded that I can only take so much stimulation and move gingerly as I moved too fast after getting home when I fetched and opened the mail, checked and responded to my emails, etc. I then had a dizzy spell for a short while. But I quickly recover and receive a clean bill of health from Sarah when she asked me to do the laundry while she goes out on errands.
This brings us to today (Tuesday, Feb. 4th). Iíve been spending all day at our desk responding to various emails, writing this diary, etc. And yet, Iím feeling okay Ė probably 80%. Iím still getting very slight dizzy spells, especially if I turn my head too quickly. My head is still slightly numb, but I have no problems touching my scar, although Iím delicate with it. Sleeping at night is still somewhat uncomfortable as I avoid sleeping on my right side. Hence, my sleeping positions are still limited. I can take a good amount of stimulation in terms of reading, writing, or watching things as long as Iím not moving my head much. Work is slow these days as Iím awaiting my next assignment. If I was currently on a project, I think I would have taken the rest of the week off anyway, especially since I would have likely been traveling for work.
Thatís all folksÖ for now. I will write a bit more in the next few days then again shortly after March 11th when I first get my cochlear implant turned on (as my head needs to heal first).
Next (Entry #3: March 25, 2003 - two weeks after CI Activation)
Back (Entry #1: January 29, 2003 - day of CI surgery)
| Entry #1 | Entry #3 | Entry #4 | Entry #5 | Entry #6 |